Kidney Failure and Transplantation: Challenges, Solutions, and the Future of Treatment
An Expert Insight by cckaam
Introduction
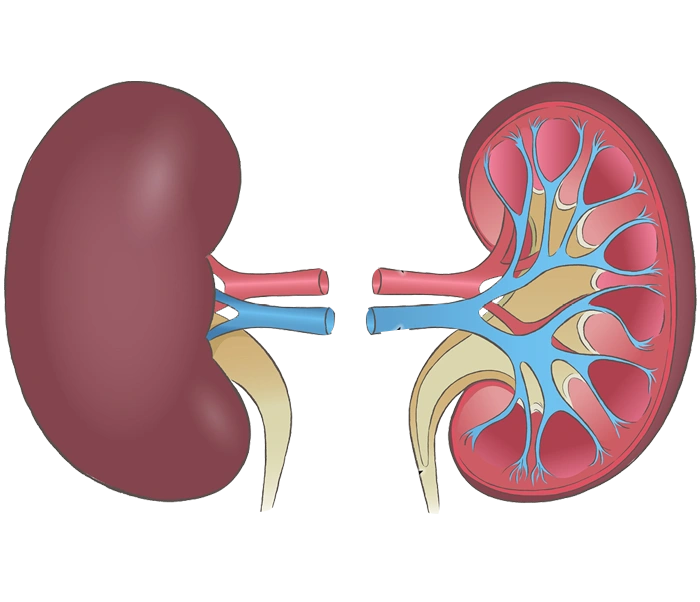
The kidneys are among the most vital organs in the human body, responsible for filtering waste products, regulating blood pressure, and maintaining fluid balance.
Kidney failure is a serious and increasingly common medical condition that can significantly affect a patient’s quality of life. In advanced stages, only two therapeutic options remain: dialysis or kidney transplantation.
This article offers a comprehensive overview of kidney failure, the transplantation process, associated challenges, and advanced treatment strategies.
What is Kidney Failure?
Kidney failure occurs when the kidneys lose their ability to perform essential functions. It can result from various causes, including:
- Diabetes
- Hypertension
- Inflammatory kidney diseases (e.g., glomerulonephritis)
- Genetic conditions such as polycystic kidney disease
- Infections and drug toxicity
Types of Kidney Failure:
- Acute Kidney Injury (AKI): A sudden and often reversible decline in kidney function.
- Chronic Kidney Disease (CKD): A gradual deterioration of kidney function over time, potentially progressing to complete failure.
Symptoms of Kidney Failure
Patients may experience:
- Extreme fatigue
- Swelling in the feet and ankles
- Decreased urine output
- Nausea and vomiting
- Persistent itching
- Uncontrolled blood pressure
- Difficulty concentrating and memory loss
Treatment Options for Kidney Failure
In advanced stages, two primary treatment options are available:
- Dialysis
Dialysis removes waste, excess salts, and fluids from the blood. There are two main types:
- Haemodialysis: Blood is filtered using a dialysis machine.
- Peritoneal Dialysis: Utilises the lining of the abdominal cavity to filter blood internally.
Limitations:
While life-sustaining, dialysis often leads to reduced quality of life and requires frequent sessions.
- Kidney Transplantation
Kidney transplantation involves replacing a diseased kidney with a healthy one from a living or deceased donor. It is considered the most effective treatment for enhancing both survival and quality of life in eligible patients.
Kidney Transplantation: Process and Phases
Patient Selection
Candidates must undergo thorough medical evaluations, including:
- Blood tests
- Tissue compatibility (HLA) testing
- Cardiac and pulmonary assessments
Donor Sources
- Living Donor: Usually a family member or a willing volunteer
- Deceased Donor: A donor declared brain-dead
Surgical Procedure
- The transplant surgery typically lasts between 3 to 5 hours.
- The new kidney is connected to the patient’s blood vessels and urinary tract.
- The diseased kidneys are usually left in place unless complications arise.
Post-Transplant Care
- Lifelong immunosuppressive medications to prevent rejection
- Regular follow-up with a transplant team
- Healthy lifestyle practices to minimise infection risks
Challenges in Kidney Transplantation
Despite being the optimal treatment, kidney transplantation is not without obstacles:
- Shortage of Donor Kidneys
One of the major barriers is the lack of available healthy kidneys, resulting in long waiting times for many patients.
- Organ Rejection
The immune system may identify the new kidney as a foreign object and attack it.
- Side Effects of Immunosuppressive Drugs
Anti-rejection medications can lead to complications such as diabetes, chronic infections, and increased cancer risk.
- Psychological Impact
Post-transplant patients may face mental health issues including anxiety, depression, or difficulty adjusting.
Strategies to Improve Transplant Success
- Early diagnosis and conservative treatment of kidney disease
- Promoting living kidney donation through education and awareness
- Use of advanced technologies such as genetic registries to enhance donor-recipient matching
- Development of safer immunosuppressive medications with fewer side effects
- Psychological counselling and robust social support for transplant recipients
The Status of Kidney Transplantation in Iran
Iran is recognised as a regional and global leader in kidney transplantation.
Renowned medical centres such as Namazi Hospital in Shiraz, Labbafinejad Hospital in Tehran, and Dr. Shariati Hospital boast high transplant success rates and cutting-edge medical infrastructure.
Iran is also one of the few countries with an organised national programme for kidney donation from both living and deceased donors, supported by professional ethics and medical transparency.
Conclusion
Kidney transplantation remains the gold standard treatment for patients with end-stage kidney disease, offering significant improvements in both longevity and quality of life.
With continuous advances in medical technology, increased public awareness around organ donation, improved immunosuppressive therapies, and psychological support, the future of kidney transplantation is more promising than ever.
If you or a loved one requires expert consultation about kidney transplantation, contact the certified transplant centres and healthcare advisors through cckaam to receive the most reliable and professional care available in Iran.
Nutrition in Kidney Failure and Post-Transplant Patients: A Comprehensive and Practical Guide
Published by cckaam – Expert Kidney Care and Transplantation Support
Introduction
Proper nutrition plays a critical role in managing kidney disease and enhancing the success of kidney transplantation.
Patients with kidney failure or those who have undergone a kidney transplant require a specialised, balanced, and medically sound diet to support kidney function, reduce medication side effects, and improve overall quality of life.
This article presents a comprehensive overview of essential dietary principles for both pre- and post-transplant kidney patients.
The Importance of Nutrition in Kidney Failure
When kidneys are impaired, their ability to filter waste, balance fluids, and regulate electrolytes diminishes. A well-planned diet can:
- Reduce stress on the kidneys
- Lower toxin build-up in the blood
- Control swelling and metabolic complications
- Slow the progression of kidney disease
Nutritional Principles for Patients with Kidney Failure
- Protein Intake Management
- In early stages of kidney disease, protein intake should be limited to reduce waste accumulation.
- Dialysis patients, however, require high-quality proteins such as lean poultry, fish, eggs, and low-fat dairy to maintain muscle and energy levels.
- Sodium (Salt) Restriction
- Limiting salt helps control high blood pressure and fluid retention.
- Recommended sodium intake: less than 2,300 mg per day.
- Potassium Control
- Elevated potassium levels can lead to serious heart problems.
- High-potassium foods (bananas, potatoes, spinach) should be restricted based on blood test results.
- Phosphorus Limitation
- High phosphorus can cause bone weakness and vascular issues.
- Foods like full-fat dairy, dark-coloured sodas, and some nuts should be limited.
- Fluid Management
- Dialysis patients often need to limit fluid intake to avoid swelling and heart strain.
Nutrition After Kidney Transplantation
After a kidney transplant, dietary priorities shift to support the new kidney, minimise side effects of immunosuppressive drugs, and prevent complications.
Post-Transplant Nutritional Goals:
- Promote tissue healing and recovery
- Reduce infection risk
- Prevent weight gain and cardiovascular disease
- Control blood glucose and blood pressure
- Increased Protein Intake
- Protein needs rise to support wound healing and tissue regeneration.
- Recommended sources: lean meats, skinless poultry, fish, eggs, low-fat dairy.
- Calorie Management
- Corticosteroids (e.g., prednisone) can lead to weight gain.
- A low-fat, low-sugar, and low-salt diet is essential.
- Sugar Limitation
- To prevent steroid-induced diabetes, intake of sweets and refined carbohydrates should be reduced.
- Sodium Regulation
- Sodium intake must remain low to manage blood pressure.
- Bone Health Protection
- Immunosuppressants can lead to osteoporosis.
- Sufficient intake of calcium and vitamin D is crucial.
Recommended Foods for Post-Transplant Patients
| Food Group | Recommended Options |
|---|---|
| Proteins | Fish, skinless chicken, lean meats, eggs, legumes |
| Dairy | Low-fat milk, yoghurt, low-fat cheese |
| Vegetables | Lettuce, cucumber, tomatoes, broccoli |
| Fruits | Apples, pears, berries, moderate amounts of watermelon |
| Grains | Whole-grain bread, brown rice, oats |
| Healthy Fats | Olive oil, avocado, unsalted raw nuts |
Foods to Limit or Avoid
- High-sodium items (sausages, processed meats, fast food)
- Sugary drinks and processed fruit juices
- Processed or packaged foods
- Sweets and desserts high in sugar
- Salted or roasted nuts
- Alcohol and tobacco (strictly prohibited)
Key Nutrition Tips for Kidney Patients
- Eat smaller, more frequent meals throughout the day.
- Drink only clean, purified water.
- Avoid raw or undercooked foods (especially meat and eggs) to reduce infection risk.
- Maintain a healthy body weight.
- Work closely with a registered dietitian and your transplant team to create a personalised meal plan.
Conclusion
Nutrition is a foundational pillar in the successful treatment and recovery of patients with kidney failure or those who have received a transplant.
Following a well-balanced diet tailored to each stage of treatment can enhance kidney function, speed recovery, and improve long-term quality of life.
Partnering with qualified nutritionists and your medical team ensures a safe and effective nutritional strategy for lasting health.